Sleep and Prediabetes: The Overlooked Link
Published on 10/3/2025 · 📖 5 min read

This article is intended for general wellness education only. It is not medical advice. Please consult a healthcare provider for any medical concerns.
Why Sleep Matters for Blood Sugar Wellness
When people think about prediabetes, the focus often lands on food choices, exercise, or weight management. But there’s another key factor that often gets overlooked: sleep quality.
Research suggests that insufficient sleep doesn’t just make you tired—it may also play a powerful role in blood sugar fluctuations, insulin resistance, and long-term metabolic health.[1][2][3]
How Sleep Loss Impacts Blood Sugar
Studies have shown that even one night of poor sleep can make it harder for the body to regulate glucose effectively. For example:
- A Lancet study found that restricting healthy adults to just 4 hours of sleep per night for six days caused their glucose response to resemble patterns seen in prediabetes.
- Research published in Diabetologia and JCEM reported that partial sleep deprivation reduced insulin sensitivity by 19–25%—meaning the body’s ability to process blood sugar dropped significantly.[2][4][5]
In other words, short or fragmented sleep may act like an invisible trigger for blood sugar spikes.
Why Does Sleep Affect Insulin Resistance?
Several biological systems connect sleep and glucose metabolism:
- Hormonal balance – Poor sleep increases cortisol (stress hormone) and reduces insulin sensitivity.
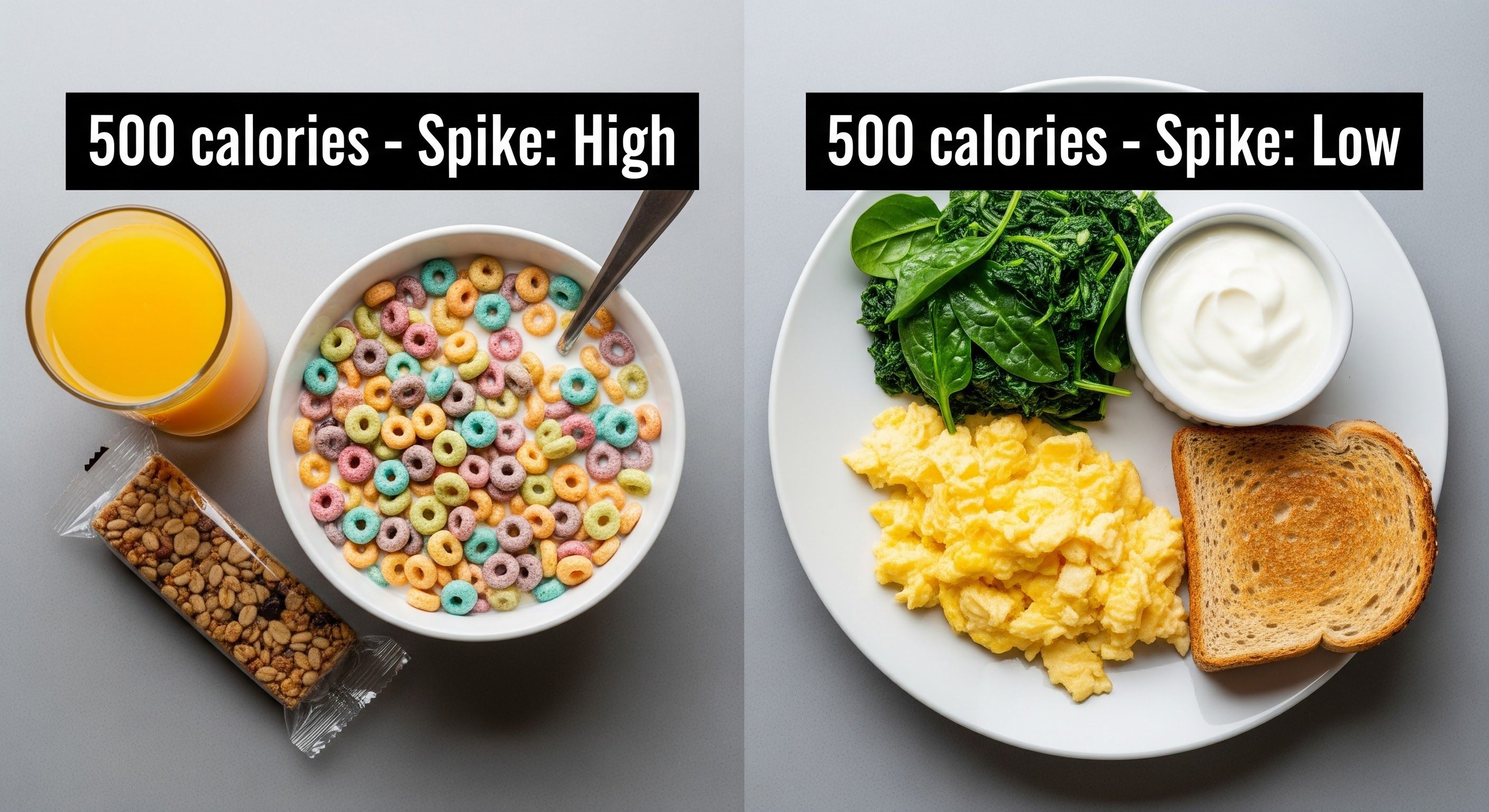
- Appetite regulation – Lack of sleep lowers leptin (fullness hormone) and raises ghrelin (hunger hormone), which may increase cravings for sugary or high-carb foods.[6]
- Circadian rhythms – The body’s “internal clock” influences when insulin works best; irregular sleep disrupts this balance.[3][7]
- Inflammation – Fragmented sleep contributes to inflammation, which has been linked to impaired insulin action.[8]
Practical Tips to Support Sleep and Blood Sugar
Improving sleep habits may help support healthier blood sugar patterns. Consider:
- Aiming for 7–9 hours of quality sleep each night.[9]
- Keeping a consistent bedtime and wake-up routine.
- Reducing screen time and blue light exposure before bed.
- Limiting caffeine later in the day.
- Eating balanced meals that avoid big sugar swings before bedtime.
- Creating a dark, quiet, and cool sleep environment.[10]
Why Sleep Awareness Matters
Many people using GlucoSpike AI notice that nights of poor sleep often lead to sharper glucose spikes the next day—even if their diet hasn’t changed. This shows how powerful sleep is in shaping daily energy, focus, and wellness.
By combining sleep awareness with mindful eating and activity, you can better understand what drives your unique blood sugar patterns.
👉 Want to see how your daily habits impact your blood sugar? Download GlucoSpike AI and start tracking your lifestyle insights today.
The Takeaway
Diet and exercise get the spotlight when it comes to prediabetes—but sleep may be just as important. Research consistently suggests that better sleep supports healthier glucose patterns, steadier energy, and long-term metabolic wellness.[5][3]
Don’t treat sleep as optional—it’s a core pillar of blood sugar balance.
Frequently Asked Questions on Sleep and Prediabetes
Q: Can poor sleep really raise my blood sugar, even if I’m not diabetic?
Yes, both experimental and observational studies show that people with poor sleep quality or shorter sleep duration are more likely to experience higher blood glucose levels—even in those without diabetes.
Q: How many hours of sleep do I need to reduce my risk?
Most research recommends at least 7–8 hours of high-quality sleep per night for optimal metabolic health. Less than six hours per night is associated with higher risk of insulin resistance and prediabetes.
Q: Does the time I go to bed affect my risk for prediabetes?
Yes; later bedtimes and irregular sleep schedules are linked to poorer glucose control and higher risk of blood sugar spikes, even after adjusting for total sleep duration.
Q: Can sleep apnea or insomnia contribute to prediabetes?
Sleep disorders like obstructive sleep apnea or chronic insomnia increase the risk for insulin resistance and consequently may trigger prediabetes, according to clinical research.
Q: Is the impact of sleep on blood sugar immediate or long term?
Both. Just a single night of partial sleep deprivation can raise blood sugar and reduce insulin sensitivity, but long-term sleep deprivation or poor sleep quality can lead to sustained metabolic problems and progression to type 2 diabetes.
Q: Does blood sugar affect sleep quality too?
Yes. High blood glucose can make it harder to fall asleep and stay asleep, while poor sleep further disturbs glucose metabolism—a vicious cycle for people at risk of diabetes.
Q: Are there specific sleep habits that matter most?
Consistent sleep routines, going to bed before midnight, and waking up at the same time every day are linked to better glucose control for people with prediabetes.
Q: What practical tips can help improve both sleep and blood sugar?
Maintain regular sleep and wake times, create an environment that encourages restful sleep, avoid screens and caffeine late at night, eat balanced meals, and treat underlying sleep disorders if present.
 GlucoSpike AI
GlucoSpike AI